Revenue Cycle Management in USA Healthcare
RCM-Introduction
Introduction
Revenue Cycle Management (RCM) is the backbone of financial sustainability in the U.S. healthcare system. From patient registration to final payment, RCM ensures that providers are reimbursed accurately and efficiently for the care they deliver. In today’s complex healthcare environment—marked by evolving regulations, payer requirements, and patient expectations—effective RCM is not just a financial necessity, but a strategic advantage.
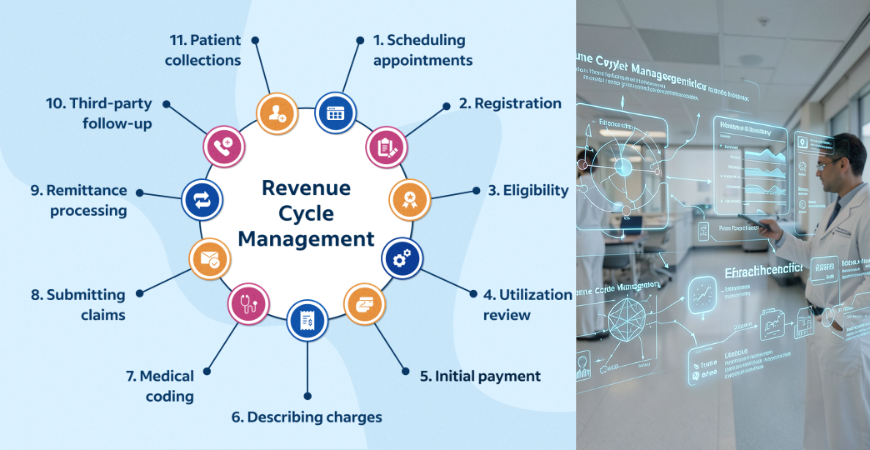
What is Revenue Cycle Management?
Revenue Cycle Management refers to the end-to-end process of managing healthcare finances, including:
- Patient Access & Registration – Collecting demographics, insurance details, and verifying eligibility.
- Charge Capture – Recording services provided with accurate medical coding (CPT, ICD-10, HCPCS).
- Claims Submission – Sending claims to payers electronically with compliance checks.
- Denial Management – Identifying, appealing, and resolving rejected claims.
- Payment Posting – Recording payments from insurers and patients.
- Accounts Receivable Follow-up – Ensuring outstanding balances are collected.
Why RCM is Critical in USA Healthcare
- High Administrative Costs: The U.S. healthcare system has one of the highest billing and insurance-related costs globally.
- Complex Payer Landscape: Multiple private insurers, Medicare, and Medicaid create diverse rules and reimbursement models.
- Regulatory Compliance: HIPAA, CMS guidelines, and value-based care models demand accuracy and transparency.
- Patient Responsibility: With rising deductibles, patient collections form a significant part of revenue.
Key Challenges in RCM
- Claim Denials: Up to 10–15% of claims face denials due to coding errors or incomplete documentation.
- Regulatory Changes: Frequent updates in CMS policies and payer rules require constant adaptation.
- Technology Integration: Many providers struggle with outdated systems or lack of interoperability.
- Patient Engagement: Educating patients about billing, insurance, and payment options is often overlooked.
Best Practices for Effective RCM
- Accurate Data Capture: Ensure patient information and insurance eligibility are verified upfront.
- Strong Coding & Documentation: Invest in certified coders and regular audits.
- Automation & AI Tools: Use RCM software for claim scrubbing, denial prediction, and workflow automation.
- Analytics & Reporting: Monitor KPIs like Days in Accounts Receivable (AR), Clean Claim Rate, and Denial Rate.
- Staff Training: Continuous education on compliance, coding updates, and payer policies.
- Patient-Centric Billing: Offer transparent statements, online payment portals, and financial counseling.
Future of RCM in USA Healthcare
- Value-Based Care: Shift from fee-for-service to outcome-driven reimbursement.
- AI & Predictive Analytics: Smarter denial management and revenue forecasting.
- Telehealth Integration: Adapting RCM workflows for virtual care billing.
- Patient Financial Experience: Enhancing transparency and affordability to improve satisfaction.
Conclusion
Revenue Cycle Management is more than just billing—it’s the lifeline of healthcare organizations in the USA. By combining technology, compliance, and patient engagement, providers can reduce denials, improve cash flow, and deliver better care experiences. For healthcare businesses, investing in robust RCM processes is not optional—it’s essential for long-term success.

Leave a Comment